The Medicaid waiver proposal the administration has drafted claims the changes will save $2.2 billion over the first 5 years of the program. But the data shows those savings would occur because fewer Kentuckians are covered — the exact problem of lack of coverage Kentucky’s Medicaid expansion has been so successful at addressing.
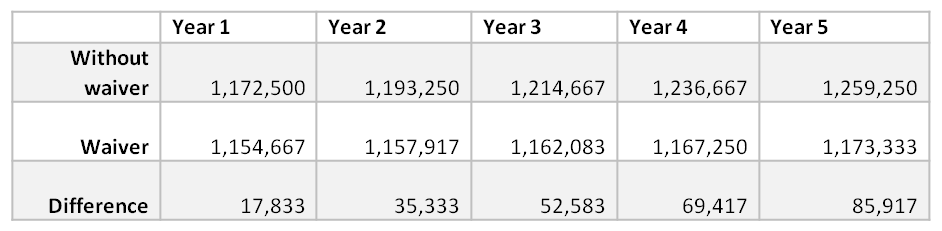
The data provided shows 17,833 fewer people will be covered by Medicaid in the first year of the demonstration compared to not having the waiver, a number that would grow to 85,917 in year 5 (data from report presents “member months,” and the table below converts that to number of members by dividing by 12) (see more on drop in enrollment here and here).
Source: KCEP calculations from Kentucky HEALTH document.
Lower enrollment is the reason for the estimated $2.2 billion in savings over the 5 year demonstration period. Other cost savings don’t explain the decline because the projected cost per member, per month is actually slightly higher for the Medicaid expansion population under the waiver, though it is slightly lower for children and non-expansion adults.
Fewer people enrolled should be expected because the proposal includes a number of measures that will reduce coverage, including denying benefits to people who don’t pay premiums and locking them out for a period of time; also locking out people who miss reenrollment deadlines; and work requirements for maintaining coverage. Ample past research shows such barriers will reduce the number of people who can participate. But the purpose of 1115 Medicaid waivers is to test ways to expand coverage or otherwise improve care, not move backwards on health care access.
The administration suggests coverage reduction will happen because they will move people to private insurance plans. But big claims around that are not realistic, and reflect a lack of understanding of the realities facing low-income Kentuckians and changes in health insurance markets.
Most of those who have gotten coverage because of Medicaid expansion are working now. But a declining share of all workers get insurance through their employers because they either aren’t offered coverage or it isn’t affordable, and stagnant wages at the bottom make it more difficult for many people to afford private insurance. Jobs are lacking in big parts of the state, and other Kentuckians face barriers to better employment including a criminal record, lack of education and training, inability to find to affordable child care and other hurdles that won’t be removed by punitive measures denying care. In fact, reducing the number of people covered will worsen health problems, lowering quality of life, driving health costs back up as people return to the emergency room and making it even harder for some Kentuckians to access work and contribute fully to their communities.