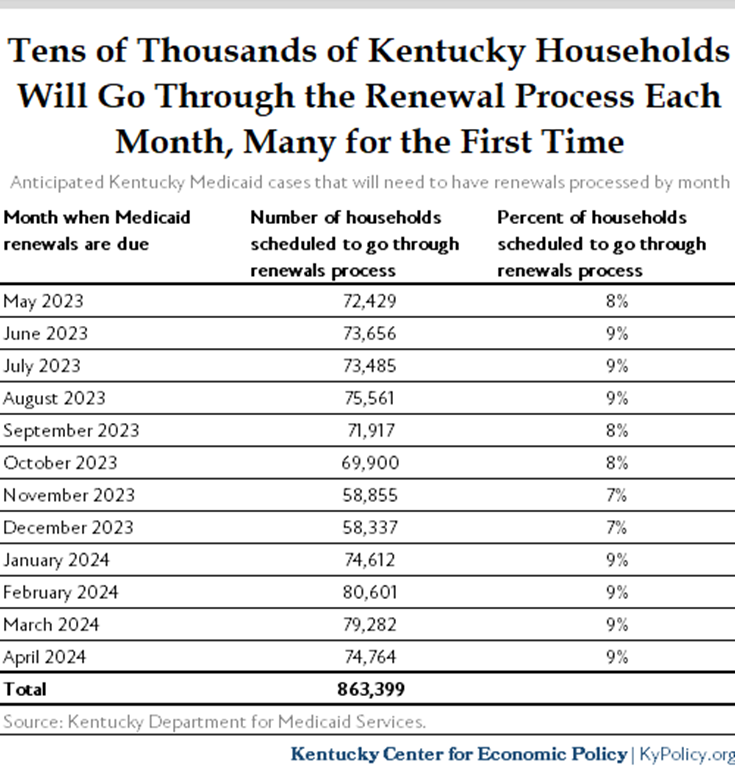
Kentucky, like every other state, is re-starting its Medicaid renewals process after a three-year pause due to the COVID-19 pandemic and ensuing downturn. During this year-long process, the state must determine eligibility of 1.7 million people in 862,000 households covered by Medicaid. An estimated 236,246 of those Kentuckians will need to take action over the next year to keep their Medicaid, or else find coverage elsewhere.
New data from the state, which it will have to report on a monthly basis, show the renewals process is now fully underway and mostly on-track. In April, the state automatically (or “passively”) renewed the coverage of 49,499 of the 72,429 households scheduled to go through the process that month, a 68% “passive” renewal rate. That’s below the 86% passive renewal rate the state expects to hit through all 12 months of renewals. The discrepancy is likely due to April’s renewal batch including a higher share of members who turned 65 since eligibility was last verified than will be the case in the months ahead. Those Kentuckians are likely eligible for Medicare now, and therefore no longer eligible for Medicaid, with some exceptions.
In addition to these passive renewals, there are 22,930 households covered by Medicaid in April’s batch that need to verify their eligibility to keep coverage. Just 1,754, or 7.6%, have completed that process so far. Of those, four out of five either recertified their eligibility for Medicaid or are getting a subsidized health insurance plan on the marketplace, with the remaining 547 determined to be ineligible. The other 21,176 active renewal cases will have until the end of May to complete the renewal process if they wish to remain covered by Medicaid. It is likely some are already insured through their job, and are simply not replying to the state because they no longer need that form of health coverage.
The state has aggressively worked to reach households that will need to take action to renew. In April, it mailed notices mid-month, sent 49,675 emails and made 52,000 phone calls to all 22,9430 of the month’s active renewal cases. Of the 22,930 notices sent out, 1,576 were undeliverable, which is why it was so important for Medicaid members to update their address through their kynect account. It remains critical for Medicaid members to ensure their address is accurate as the state moves through the rest of the cases. If the state doesn’t hear back from those who will need to actively renew by mid-May, they will begin another round of phone calls.
This month was just the beginning of the renewal process, and the state will continue to reach out to those who need to provide information to renew – which they will have 12 months to initiate and 14 months to complete. Ideally, the state will pursue a higher passive renewal rate moving forward, ensuring as few people lose coverage as possible.