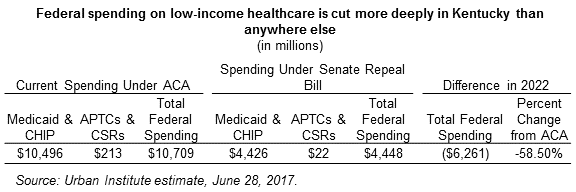
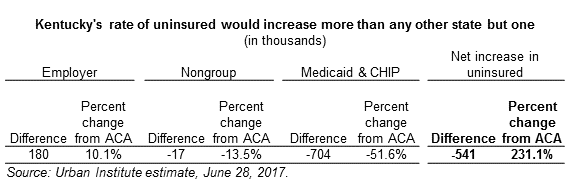
Kentucky would see its uninsured rate more than triple under the proposed Senate bill to repeal the Affordable Care Act (ACA). According to the Urban Institute, Kentucky’s uninsured population would jump by 541,000 people in 2022 based on the proposed changes to the healthcare system. The primary reason for the coverage losses is a cut in federal funding for Medicaid and premium subsidies on the insurance marketplace of $6.3 billion in 2022, a 58.5 percent reduction. That’s the largest percentage cut of any state.
The coverage losses under the Senate bill come from 704,000 Medicaid enrollees and 17,000 marketplace enrollees losing coverage. The Urban Institute also estimates that 180,000 Kentuckians would gain coverage through their employer, though if Kentucky decides to waive the Essential Health Benefits, these individuals would be enrolled in inferior coverage that would also be subject to annual or lifetime caps.
The percent of Kentuckians under Medicaid who would lose coverage is particularly alarming. In cutting the number of people covered by Medicaid in half, the Senate repeal bill kicks a higher share of Kentuckians off Medicaid than anywhere else. This is such a large share of Kentucky’s population that it essentially strips insurance from 1 in 6 Kentuckians.
The effort to roll back the Affordable Care Act and then permanently squeeze funding for traditional Medicaid does not just take us back to the days before the ACA improved Kentuckians’ health coverage. It sets the commonwealth back even further and jeopardizes the substantial health care gains we’ve made over the past three years. It would also pull billions of federal dollars from our economy, which is still in recovery from the recession. No matter which version of ACA repeal you look at, the results are the same – a catastrophe for Kentuckians’ health and our economy.