Many of Kentucky’s 1.4 million Medicaid enrollees would lose coverage from the radical cuts proposed in the American Health Care Act (AHCA) and the proposed Trump Budget. Because of the changes in the AHCA to the marketplaces, those left without Medicaid coverage wouldn’t have other affordable options for insurance, either. This toxic combination of slashing Medicaid and making private insurance more expensive will hit older and low-income Kentuckians especially hard.
According to a report by the Center on Budget and Policy Priorities, a large number of people near the poverty line will likely become uninsured as a result of large cuts to Medicaid, and then face prohibitively expensive private insurance plans.
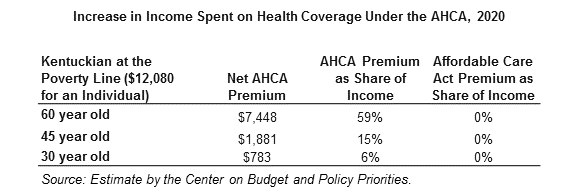
The table below shows the increase in health care coverage costs, as a share of income, for individuals at the poverty line. Costs would skyrocket for low-income Kentucky seniors, especially, who would see coverage costs rise to nearly 60 percent of their total income. But even for a 30 year old living at the poverty line, a 6 percent, or $783 annual increase, (more than monthly fair market rent for a one bedroom apartment anywhere in Kentucky) in his or her total personal budget of $12,080 per year would not likely be manageable.
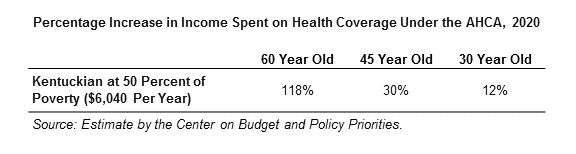
The picture becomes even bleaker for extremely low-income Kentuckians – those at half the poverty level ($6,040 for individuals). For a 60 year old Kentuckian, marketplace changes in the AHCA would mean the cost of coverage would cost more than he or she earns in a year.
The mechanisms by which insurance costs increase are numerous: at the heart of the AHCA is a massive cut to traditional and expanded Medicaid. Prior to the expansion in 2014, Medicaid was very restrictive in who could get covered, which is why allowing Kentuckians with a higher income to participate resulted in nearly half a million more getting covered. The AHCA sets Kentucky’s health back by ending the expansion, and then goes even further by making permanent and ongoing cuts to the traditional Medicaid program as well.
On top of those reductions in Medicaid coverage, the AHCA makes changes to the marketplace that increase health care costs for individual insurance policy holders in a few ways:
- Moving from income-based to less generous age-based assistance for paying premiums.
- Allowing insurers to charge older people up to five times more for coverage than younger people (as opposed to three times more under current law).
- Repealing the Cost Sharing Subsidies, which help reduce out-of-pocket costs for low-income marketplace enrollees.
- Allowing insurers to pay less of an enrollee’s total healthcare costs. The CBO estimates insurers will pay 65 percent on average versus the current average of 70 percent.
Combined, these Medicaid cuts and the individual marketplace changes would mean that for the hundreds of thousands of newly uninsured Kentuckians, there will be nowhere to turn for coverage; a perfect storm creating a devastating setback for the health of the commonwealth.