A recent evaluation of Indiana’s Medicaid waiver program should stand as a warning for Kentucky policymakers attempting to similarly charge premiums in our own Medicaid program. While proponents of Kentucky’s Medicaid waiver proposal say charging premiums wouldn’t be a barrier to coverage and care for low-income Kentuckians, the findings of the study of Indiana’s waiver suggest otherwise.
One aspect of Indiana’s Medicaid waiver program, “Healthy Indiana Program 2.0,” (HIP 2.0), is a requirement that enrollees make monthly contributions to a type of Health Savings Account called a POWER Account. The consequences of not making these contributions differ based on income:
- Members with income above the poverty line are disenrolled from Medicaid altogether and locked out of the program for six months.
- Members with income below the poverty line are moved from the standard policy, HIP Plus, into HIP Basic, a much more limited plan with co-pays.
The recent evaluation sought to find out how well Hoosiers were making their mandatory monthly POWER Account Contributions (PACs), and what was happening to those who didn’t. Here’s what the study found and the implications for Kentucky:
Many low-income Hoosiers were left without coverage because they didn’t pay in.
During the first 21 months of the waiver program, 324,840 (55 percent) of the 590,315 people eligible to pay PACs didn’t make a required payment at some point. All of them were then kicked off of Medicaid or were left with inferior coverage:
- Among Medicaid enrollees above the poverty line, 13,550 were disenrolled and 46,176 who qualified and applied for coverage were not enrolled because they did not pay. Combined, this rejected group represents 29 percent of those who qualified and applied for Medicaid with incomes above the poverty line.
- Among Medicaid enrollees below the poverty line, 286,914 were given HIP Basic coverage because they didn’t make a PAC. Of these, 40,756 made at least one PAC, but missed a payment and as a result were moved from HIP Plus to HIP Basic coverage.
People didn’t make their PAC for many reasons, but the most common were that people could not afford the contribution, were confused about the payment process or didn’t know they were required to make a payment.
Among Medicaid enrollees above the poverty line who were kicked off of coverage because they didn’t make a PAC:
- 44 percent said they couldn’t afford the contributions.
- 17 percent said they were confused by the payment process.
- Around one percent said they didn’t know a payment was required.
Among Medicaid enrollees above the poverty line who qualified for HIP Plus coverage but were never enrolled because they failed to make a PAC:
- 22 percent said they couldn’t afford the contributions.
- 22 percent said they were confused by the payment process.
- 8 percent said they didn’t know a payment was required.
Among Medicaid enrollees below the poverty line who were moved to HIP Basic coverage because they missed a PAC:
- 34 percent said they couldn’t afford the contributions.
- 17 percent said they were confused by the payment process.
- 25 percent said they didn’t know a payment was required.
The number of people either moved to HIP Basic or left without coverage might have been even higher except that employers and non-profits stepped in and paid for 5,770 people’s PACs, or roughly 2.5 percent of the HIP Plus enrollees. This practice, which will be allowed under Kentucky’s proposed changes to Medicaid, may mask the true affordability of premiums for some low-income persons.
Some people who were kicked off HIP coverage or who qualified but were never enrolled due to PAC non-payment were able to get some form of insurance: 47 percent of people kicked off and 41 percent of people who were never enrolled had coverage when surveyed. But that means that 53 to 59 percent were without health care coverage of any kind.
People who were kicked off coverage or never enrolled found it harder to get to the doctor.
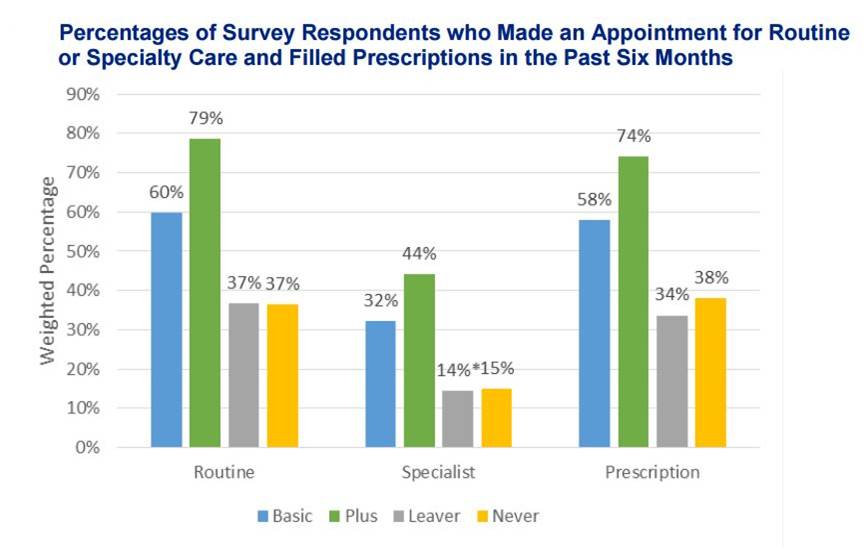
Both HIP Basic and Plus members were more likely to have received routine care, have seen a specialist, or have had a prescription filled than people who were kicked off coverage or never enrolled.
Source: Lewin Group, “Healthy Indiana Plan 2.0: Power Account Contribution Assessment,” March 21, 2017.
This stands in stark contrast to the common claim that people who have Medicaid coverage are less likely to be able to access health care. It also shows people were less likely to get needed health care because of failing to pay their PAC.
Kentucky’s premiums are similar, so we can expect similar results.
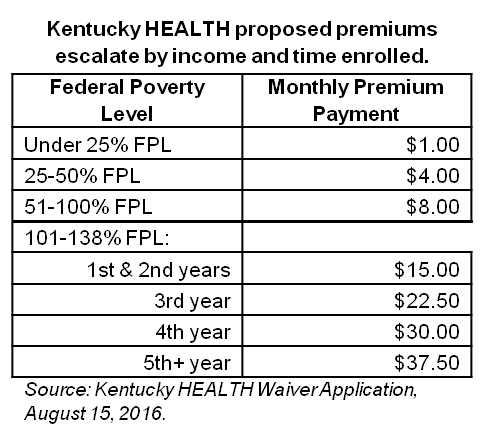
Proposed changes to Kentucky’s Medicaid program, through a similar waiver process, include premiums for most enrollees. These premiums are based on income for all enrollees, and also on the length of time enrolled in Medicaid for enrollees above the poverty line. Much like HIP 2.0, Kentucky HEALTH, as the waiver is called, would drop people into more limited coverage if they are below the poverty line and fail to make premiums. Those above the poverty line would be locked out for six months unless they paid back three months’ worth of premiums and took a financial or health literacy class. The Kentucky waiver is even harsher than HIP 2.0 in that people earning above the poverty line would face rising premiums over time.
Given the findings of the HIP 2.0 evaluation, we can expect large numbers of Kentuckians to be left without coverage if the waiver is approved by the federal Department of Health and Human Services. The assessment of the Indiana waiver confirms that both the cost and process of paying premiums is a barrier to coverage for low-income people. It also shows us that when Medicaid-eligible people are left without coverage they don’t see the doctor or get prescriptions filled as often. If we really care about people being insured and getting healthier, Indiana is a perfect example of what not to do..