As a result of factors contributing to the state’s poor health, Kentucky is especially vulnerable to the health and economic impacts of the COVID-19 pandemic. A new annual report from Robert Wood Johnson Foundation’s County Health Rankings and Roadmaps provides data about the relatively large share of Kentuckians already in poor health and who are at a higher risk of serious complications from the coronavirus.
When compared to other states, Kentuckians are at a higher risk of COVID-19 becoming a serious illness, over 45% of people older than 60 and over 20% of adults under 60 would see serious health complications if they contracted the disease. Policies that address underlying health factors leading to these poor outcomes, and that mitigate the severity of the current public health crisis, will also make Kentuckians healthier in the long term.
According to the new data, 24% of Kentucky adults report fair or poor health (the lowest-possible self-reported health status), compared to 17% nationally. Kentuckians also reported feeling physically unwell an average of 5.1 days per month and mentally unhealthy an average of 5 days per month, compared to 3.8 physically unhealthy days and 4 mentally unhealthy days a month nationally.
Additionally, Kentuckians are not meeting their full potential life expectancy. The state has a high incidence of premature death at 9,700 per 100,000 people under the age of 75 compared to 6,900, nationally. This high premature death rate is largely due to preventable diseases, such as diabetes, which has been identified as a risk factor for more serious complications related to COVID-19. In Kentucky, about 13% of adults have diabetes, ranging from 8% of adults in Crittenden, Hart, Pendleton, Scott and Warren counties to 25% of adults having diabetes in Robertson County.
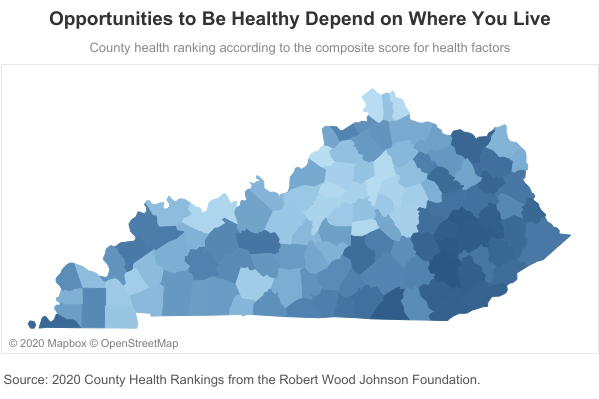
Some Kentucky counties have better health outcomes overall than others, as shown in the map below.
Research finds that many factors influence the opportunities people have to be healthy, and these can be categorized broadly as health behaviors, clinical care, social and economic factors, and the physical environment. About 40% of health challenges result from social and economic factors such as lacking access to healthy foods and low availability of good paying jobs and affordable housing.
Clinical care makes up another 20% of health outcomes, which includes access to health care and insurance coverage. And the remaining contributors to Kentuckians’ health outcomes are health behaviors and the physical environment. As respective examples of these categories, 25% of Kentuckians are current smokers compared to 17% nationally and our average air pollution (particulate matter micrograms per cubic meter) is 10.7 compared to the national average of 8.6 with some communities lacking access to clean water.
Reflecting the fact that economic factors play a big role, the map below shows where counties rank in terms of their opportunities to be healthy. Kentuckians living in the golden triangle, for instance – where there are more employment opportunities and typically higher wages – have greater opportunities for good health.
In order for Kentucky to boost the health factors that will shape how well we fare in the COVID-19 pandemic, state and federal action should be taken to:
- Make significant enhancements to Unemployment Insurance to ensure the increasing number of people experiencing layoffs have the cash they need to pay for necessities like medicine, food, and rent.
- Expand access to adequate nutrition for people who are food insecure, particularly children and older adults.
- In addition to the extended 3 month recertification period for all public assistance programs, continue to create administrative flexibilities in Medicaid and other safety net programs to minimize barriers related to in-person meeting requirements, deadlines and required documentation.
- Suspend the Public Charge rule that discourages lawfully-abiding immigrants from seeking public assistance and health care services.
- Ensure our public health departments, which have experienced a 34% decrease in staff since 2012, are adequately funded; and remove the threat of a massive increase in their pension contributions.
These emergency responses are needed to reduce transmission and the impact of COVID-19, but also to improve the underlying health factors that influence health outcomes more generally.