Despite claims that Kentucky’s coverage gains were not met with access to care and better health, several recent reports and other data show quite the opposite is true. The well documented decline in the share of Kentuckians without health insurance is already reaping other rewards.
Access to care is increasing
Kentuckians are able to get to the doctor more than before. According to a recent Commonwealth Fund ranking of state health systems, Kentucky jumped from 47th in the country to 39th between 2013 and 2015, in large part because healthcare access and affordability both grew:
- Adults who went without care because of cost dropped 34 percent.
- Adults with a usual source of care increased by five percentage points.
- Low-income, at-risk adults who went without seeing a doctor dropped by four percentage points.
A report by the Harvard School of Public Health showed that along with increased coverage among Medicaid eligible adults in Kentucky and Arkansas (states that expanded Medicaid eligibility), access to care also grew more than in Texas, which did not expand Medicaid. Several measures showed that these expansion states outpaced the non-expansion state:
- Access to a primary care doctor increased 12 percentage points.
- Regular care for chronic conditions among Medicaid eligible adults in Kentucky and Arkansas grew by 12 percentage points.
- There was a 12 percentage point decline in skipping medications due to cost.
- Reports of receiving poor or fair quality healthcare declined by 7 percentage points.
The final of a series of reports by SHADAC (commissioned by the Foundation for a Healthy Kentucky) outlining the implementation of the ACA in Kentucky showed several improvements in access for Medicaid expansion enrollees between the first quarter of 2014 and the third quarter of 2016:
- Quarterly colorectal screenings for cancer increased from 3,152 to 5,550, a 76 percent increase.
- Breast cancer screenings per quarter rose from 5,453 to 8,920, a 64 percent increase.
- Preventive dental services rose from 19,340 to 33,782, a 75 percent increase.
- Hepatitis C screenings grew from 1,208 to 4,011, more than tripling (which is important as the CDC found many Kentucky counties at risk of a Hepatitis C breakout).
- Substance Use Disorder treatments grew tremendously from 1,504 to 12,319, a 719 percent increase.
- Similarly, diabetes screenings grew from 442 to 3,579, a 710 percent increase.
More generally, the SHADAC report showed that access to care has grown among Kentuckians. Between 2012 and 2015
- There was a five percentage point increase in the share of Kentuckians who reported visiting a healthcare provider last year.
- Even as the number of people receiving healthcare coverage increased, the share of all Kentuckians who said they could find a provider that took their insurance held steady at just under 98 percent. This suggests that access to care did not, in fact, decline with the increase in number of people covered.
Health outcomes are improving
Results from these three reports also showed that as people have gotten insurance, their health has improved as well. The Commonwealth Fund ranking reported that between 2013 and 2015:
- Breast cancer deaths per 100,000 dropped from 23.4 to 20.9.
- Infant mortality deaths per 100,000 dropped from 7.2 to 6.4.
- Hospital admissions for pediatric asthma per 100,000 dropped from 167 to 117.
Similarly, the Harvard study reported health improved more for Medicaid eligible adults in Kentucky and Arkansas than in Texas:
- There was a five percentage point increase in adults who reported having excellent health.
- Although not a direct measure of health, there was a six percentage point decline in people using the emergency room. This could be because people are no longer using it as a normal source of care, and it could mean that people’s conditions are not worsening to the point where they need emergency care.
The SHADAC report showed several areas that demonstrate improved health outcomes between 2012 and 2015:
- Hospital admissions per 100,000 for asthma-related conditions fell from 68 to 58.
- Hospital admissions per 100,000 for hypertension (high blood pressure) fell from 58 to 44.
- The share of Kentuckians who smoke dropped 2.3 percentage points from 28.3 to 26 percent.
Providers are getting paid
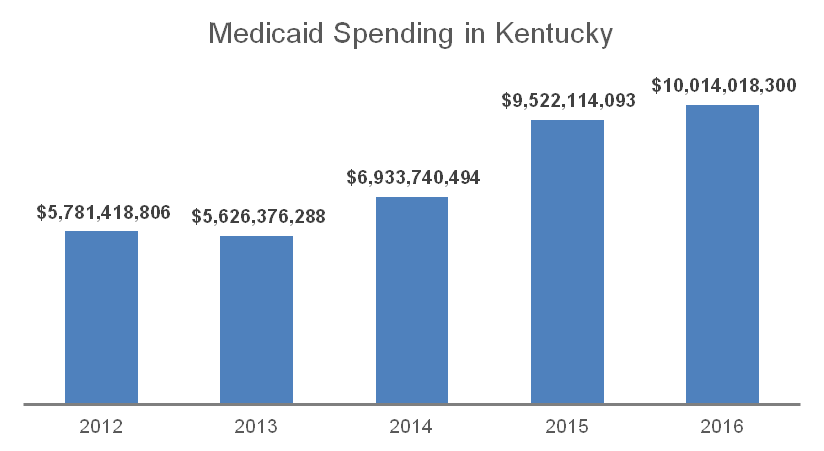
Another important measure for how coverage is translating into care is how much money is being spent on providing health services. Kentucky spent nearly $5.8 billion in 2012 to pay for care given to Medicaid enrollees. By 2016 that amount had risen to $10 billion, and covered over 400,000 more people. Most all of those dollars went to hospitals, clinics, pharmacies, long-term care facilities, and many other kinds of healthcare providers.
Source: Data from the Kentucky Office of the State Budget Director.
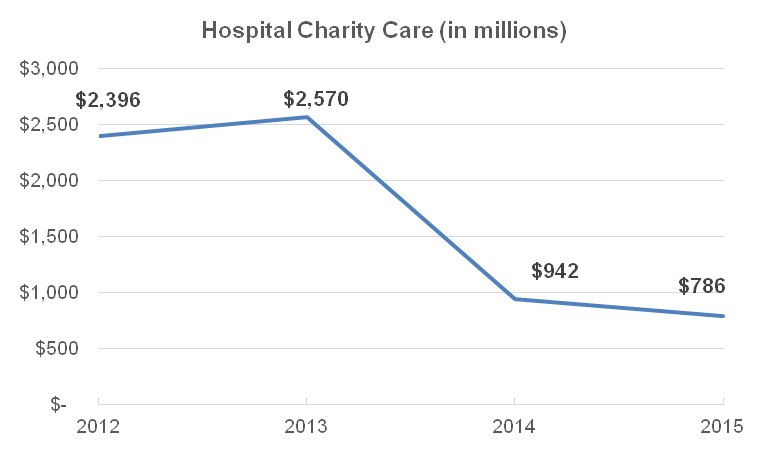
This influx in funding has made a huge difference for providers who otherwise might not have been paid for the care they offered. While there has been an increase in people receiving care, there has also been an increase in patients who can pay for their care. Uncompensated, or charity care has dropped 67 percent since 2012 according to SHADAC.
Source: SHADAC “Final Report: Study of the Impact of the ACA Implementation in Kentucky.”
Coverage is not an end goal in and of itself, but it does help people get to a doctor when they need to, which in turn helps to improve health. It is clear that Kentuckians have used the coverage they gained to get to a doctor, and there is already evidence of improved health outcomes. Stripping coverage away from 24 million Americans, including hundreds of thousands of Kentuckians, will make healthcare access much worse. Instead, lawmakers should be pursuing ways to build on our coverage gains and ensure everyone can affordably see a doctor when needed.