Medicaid is the backbone of health care in Kentucky. Along with the Kentucky Children’s Health Program (KCHIP), it provides life-sustaining medical coverage to nearly 1.5 million Kentuckians and injects tens of billions of dollars into local economies.
Yet, in an effort to partially offset the cost of massive tax cuts for America’s wealthiest individuals and corporations, Congress is moving toward deep cuts in Medicaid that would severely undermine its health, economic and fiscal benefits in Kentucky.
Medicaid provides a wide range of care for nearly a third of Kentuckians in communities across the state
Medicaid is the single largest payer of health care in Kentucky. It provides coverage for 44% of births, 16,650 of the 21,050 long-term care residents, and one in five seniors, who use Medicaid as a supplement to their Medicare coverage due to their low, often fixed incomes. Medicaid also provides home and community-based care for 31,300 Kentuckians with intellectual and developmental disabilities, brain injuries, or who require medical machines like a ventilator to live. Additionally, it insures a significant portion of the workforce, with nearly 250,000 low-wage Kentucky workers receiving health coverage through Medicaid.
There are many ways Kentuckians become eligible for Medicaid, but they generally fall into four categories:
- Disabled adults, low-income seniors and pregnant/new mothers make up most of those who have traditionally been eligible for Medicaid. As of December 2024, there were 376,900 of these Kentuckians.
- All other adults whose income is below 138% of the poverty level ($21,597 for an individual) are eligible due to the state’s 2014 Medicaid expansion. There are 478,900 Kentuckians who fall into this category.
- Children traditionally eligible for Medicaid based on an illness or disability, or due to their family income. There are 491,900 children covered by Medicaid in this way.
- For kids whose family income is slightly above Medicaid’s cutoff, KCHIP provides many of the same benefits, has similar requirements as traditional Medicaid and is administered through Kentucky’s Medicaid program. There are 133,000 such kids in Kentucky.
At the county-level, the share of the population covered by Medicaid varies greatly, from 17.9% in Spencer County to 68.8% in Owsley County.
Medicaid is good for Kentuckians’ health
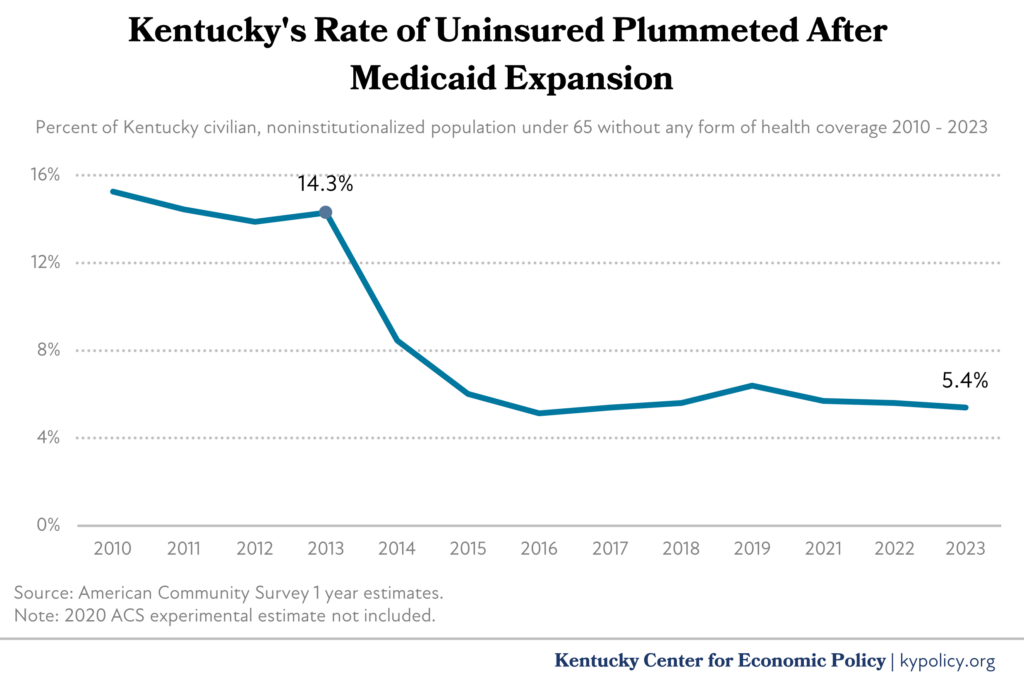
Health coverage leads to better health outcomes, and Medicaid is no exception. While traditional Medicaid has covered hundreds of thousands of Kentuckians since it was created in 1965, the 2014 expansion of Medicaid eligibility profoundly reduced Kentucky’s rate of uninsured from 14.3% in 2013 to 5.4% by 2023.
Medicaid has helped address the racial disparity in health coverage in Kentucky. In 2013, Black Kentuckians had an uninsured rate of 17.6% compared to white Kentuckians’ 13.2%, but by 2023 both had shrunk, with a smaller disparity, at 7.1% and 4.4% respectively. Medicaid plays an outsized role in Black health coverage especially – where around 30% of white and Asian Kentuckians are covered by Medicaid, 57% of Black Kentuckians are due to lower incomes.
A broad array of research using the expansion of Medicaid in states across the country as natural experiments found overwhelming evidence for its benefit on health outcomes. These include cancer diagnosis and treatment, successful organ transplant rates, smoking cessation, improved behavioral health (including substance use disorders), inpatient hospital mortality and unnecessary hospitalizations for conditions like hypertension and asthma.
Children especially benefit from Medicaid coverage. A suite of services known as “Early, Periodic Screening, Diagnostic and Treatment” are aimed at identifying and treating conditions early in life that can worsen over time and become more difficult and expensive to treat later in life.
Kentucky specifically has seen a large increase in HIV screenings, mammograms, colonoscopies, pelvic exams, preventative dental services, and diabetes screenings following Medicaid expansion. One researcher compared Medicaid enrollees in Kentucky and Arkansas, which also expanded Medicaid, to similar people in Texas, which didn’t, and found that Medicaid led to better adherence to prescribed medications, more routine care for chronic conditions, more preventative health visits, and greater self-reported excellent health.
Medicaid is good for Kentucky’s economy
By 2026, Kentucky will spend over $20 billion on health care through Medicaid mostly with federal funds and almost exclusively for health care services (Kentucky’s administrative overhead for Medicaid is 2.2%). This spending flows into communities across the commonwealth through the care received there, and then ripples throughout the economy as providers spend their pay, generating further economic activity of $1.35-$1.80 per dollar invested through Medicaid.
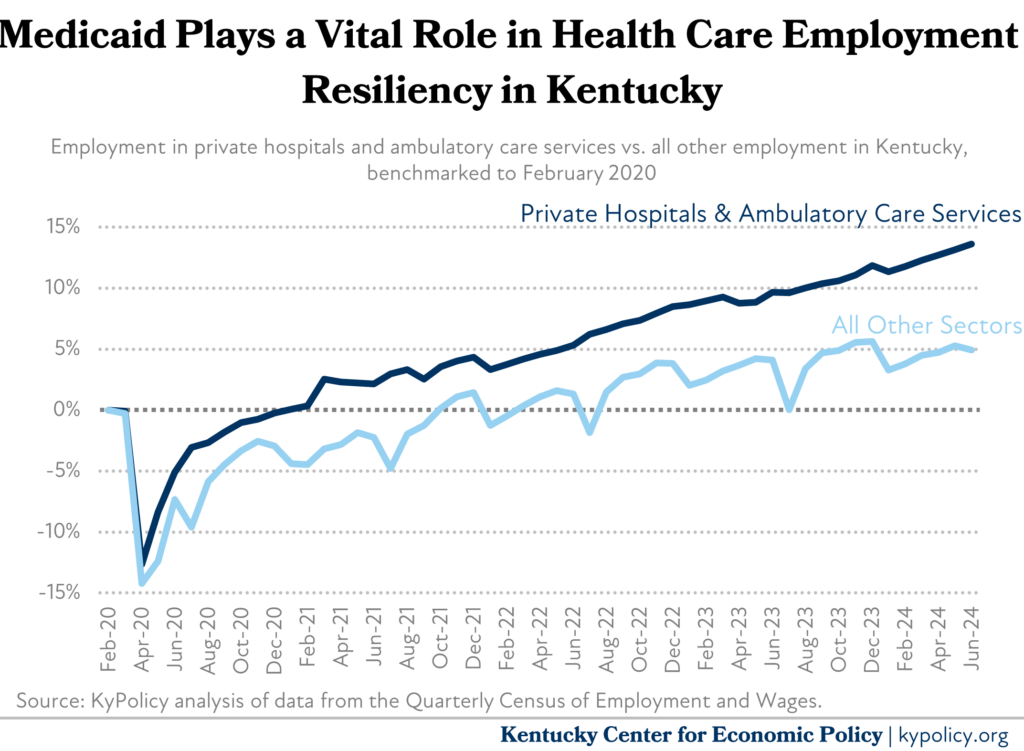
Medicaid also significantly supports employment. In private, for-profit Kentucky hospitals, Medicaid comprised 25.4% of revenue in 2023. Because of this steady revenue stream, hospital and ambulatory health care services were able to recover from the COVID-19-induced downturn much faster than the rest of the economy and grew at a faster pace.
Medicaid is a great deal for Kentucky’s budget
Crucially, Medicaid is a shared state and federal program with the federal government paying for the majority. It pays approximately 71.5% of the cost for traditional Medicaid (the program eligibility rules prior to the 2014 expansion, as mentioned above), 80% for KCHIP, and 90% for Medicaid expansion. In total, the federal government spent $14.3 billion for Medicaid while Kentucky spent just $2.4 billion in General Fund monies (and an additional $1.5 billion in restricted agency funds) – a nearly four-to-one ratio.
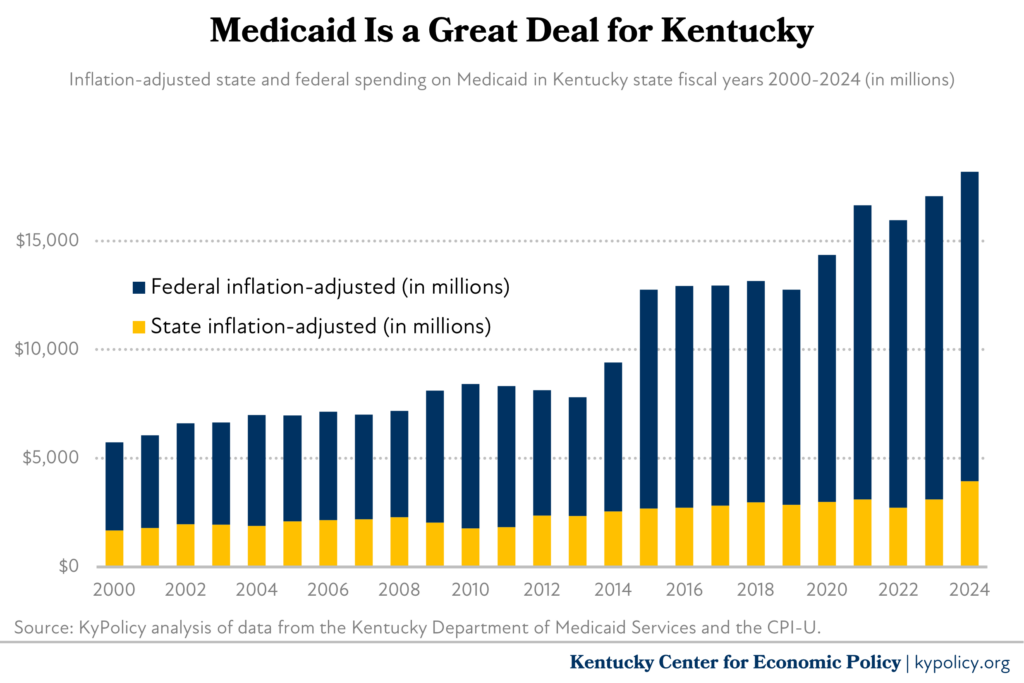
For private and university hospitals, it is an even better deal. The reimbursements for care that Medicaid pays to providers are traditionally lower than what private insurance companies pay them. But in recent years, new “state directed payment programs” use a special tax on providers to draw down enough federal funds to offer $4.5 billion in 2024 for additional payments to hospitals, bringing Medicaid’s reimbursement rates in line with commercial insurance rates.
This support and others through Medicaid have been especially helpful for rural hospitals. Consistently, in states that maximize their Medicaid program through adopting Medicaid expansion, rural hospital operating margins are larger than in states that haven’t, and are at a lower risk of closure. The role that Medicaid plays in Kentucky’s rural hospitals is especially important, as Kentucky has the sixth largest rural population in the country proportionately, and is in the top 10 for the most children, non-elderly adults and seniors covered by Medicaid.
Congress should protect Medicaid
Medicaid is a huge benefit to Kentucky’s health, economy and state budget. But the potential cuts to Medicaid that Congress is considering would undermine those gains, leaving many Kentuckians without coverage unless the state were to take on billions more in funding obligations. There is more to lose in Kentucky than in most states, and our congressional delegation should honor that risk by protecting Medicaid from any cuts.




