Recent news that the U.S. Department for Health and Human Services (HHS) will extend the COVID-19 Public Health Emergency (PHE) past July means Kentuckians with Medicaid will continue to have health coverage through November 1, 2022 without needing to take action. However, it also means that Kentuckians receiving food assistance through the Supplemental Nutrition Assistance Program (SNAP) will miss out on an extra $100 a month in grocery money through at least November because of Senate Joint Resolution (SJR) 150, which was passed during this year’s legislative session. At a total cost to Kentucky of $50 million a month, that’s $350 million less between now and November than would otherwise come to the state to fight hunger.
Kentuckians receiving help with groceries through SNAP will lose at least $350 million
In March of 2020, Congress acted to alleviate hunger during the depths of the pandemic and subsequent downturn by providing the maximum SNAP benefit amount per person rather than the normal pro-rated amount based on income. This “Emergency Allotment” (EA) was worth roughly $100 per person and over $50 million for the state per month (approximately a 41% increase). These EAs were conditional on the federal PHE as well as a state-level emergency declaration related to COVID-19. From March 2020 through April of 2022, SNAP EAs brought nearly $1.3 billion into the state to help Kentuckians avoid hunger.
But SJR 150 ended the Kentucky emergency declaration related to COVID-19 and barred the executive branch from acting on past declarations in any way, preventing the Department for Community Based Services from accepting the funding for EAs. The U.S. Department of Agriculture, which administers SNAP, will continue to provide EAs until the month following the expiration of the federal PHE, which means the final month may be in November 2022 at the soonest. If not for SJR 150, Kentucky could have received the extra SNAP funding from May to November — roughly $350 million. Because of SJR 150, SNAP benefits are being cut at a time when food costs are rising quickly.
Thanks to the expected federal PHE extension, Medicaid enrollees will get to keep their coverage for longer if they want to
Also in March 2020, Congress passed legislation increasing the federal share of traditional Medicaid spending (not expanded Medicaid) by 6.2 percentage points, saving Kentucky over $1.3 billion since then. But this increased funding came with the condition that states not remove anyone from Medicaid unless they pass away, move out of state, or ask to be removed — a provision known as the Maintenance of Effort (MOE).
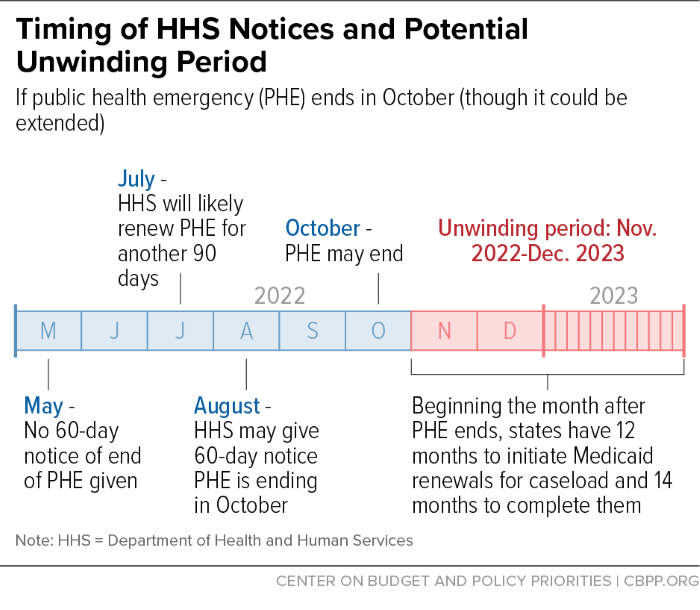
Since that time, hundreds of thousands of Kentuckians have been able to use Medicaid for their medical care and prescriptions without having to jump through the normal hoops related to renewals thanks to the MOE. This protection will remain in place until the end of the month in which the PHE expires, meaning Medicaid enrollees have until November 1, 2022 before needing to begin their renewal process at the earliest (the 6.2 percentage point increase, however, continues through at least the end of the year). The Kentucky Department for Medicaid Services estimates there are a little over 175,000 individuals who will need to provide documentation at that time to show they are still eligible, or else find coverage elsewhere. In the meantime, there are many important steps the state should begin taking now to prepare for this process and avoid unnecessarily leaving Kentuckians without coverage.