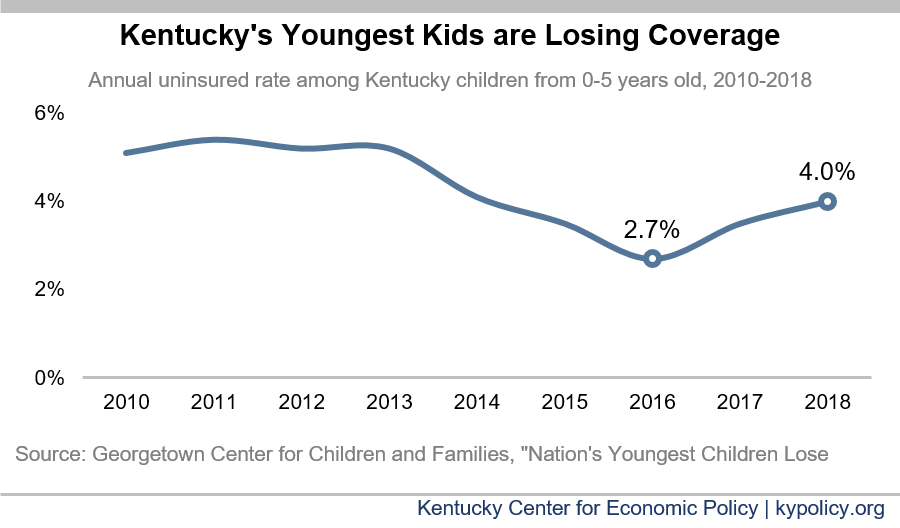
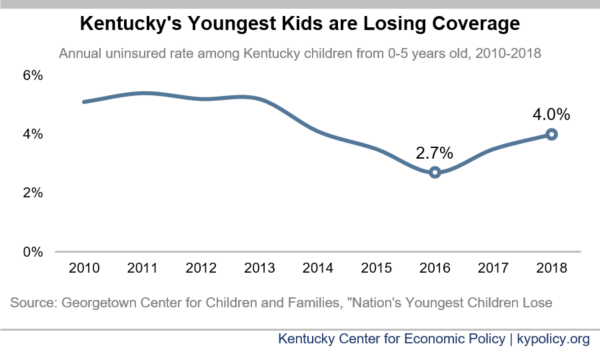
Kentucky is 3rd-worst in the nation in its alarming recent rise in uninsured children below the age of 6. According to an analysis of the most recent census data by the Georgetown Center for Children and Families, the number of uninsured children in Kentucky rose from 8,608 in 2016 to 12,973 in 2018 — meaning 4,365 more young kids don’t have health coverage. The rate of uninsured grew from 2.7% to 4%.
This decline in the number of young Kentuckians with insurance is in line with the broader coverage losses experienced in Kentucky between 2016 and 2018. But the increase in the number of uninsured young children (50.7%) far outpaced the increase in the number of uninsured Kentuckians as a whole (10.9%).
When parents began signing up for insurance through Medicaid and the exchanges after the coverage provisions of the Affordable Care Act went into place, many kids who were already eligible for coverage but uninsured also gained coverage – this phenomenon was known as the “welcome mat” effect. It is not immediately clear if the recent decline in insured children is specific to any one type of coverage. Recent policy choices may have contributed to an “unwelcome mat” effect, when families of children eligible for coverage, particularly Medicaid and KCHIP, do not apply because they are led to believe they’re not eligible or lose coverage because of paperwork requirements. Several recent policy changes may have contributed to this unwelcome mat effect:
- The 2017 ACA repeal effort at the national level and the proposed barriers to Medicaid coverage through an 1115 waiver on the state level surely sowed confusion about who was eligible for Medicaid.
- Drastic cuts of 90% to outreach and enrollment for health coverage at the federal level meant many families were unaware that they qualified for public coverage options, and may not have had adequate assistance in enrolling for coverage.
- The Public Charge rule that penalizes legally-abiding immigrant families from eventually naturalizing or even being able to stay in the United States if using certain public assistance, including Medicaid. Even before it went into effect and after it was blocked in court, it still had a chilling effect on Medicaid enrollment.
- Practices in Kentucky that enforced stricter paperwork requirements, which led to 97,438 Kentuckians losing Medicaid coverage in state fiscal year 2019. Although it’s not clear how many of these would not have been eligible had they presented the paperwork in time, how many were children or how many may have regained coverage since, an enrollment loss of that magnitude must have contributed to the increase in uninsured to some degree.
Health coverage is important for all of us, but it has outsized benefits for young children, whose early development sets the trajectory for their lifelong well-being. The American Academy of Pediatrics recommends 15 check-ups in the first 2 years of life to immunize children and catch conditions and developmental delays early while they’re more easily treatable and before they cause problems later in life. Medicaid especially has a suite of screenings and treatments known as Early and Periodic Screening, Diagnostic and Treatment (EPSDT), which is associated with a long list of immediate and lasting health benefits.
The children losing coverage will not have access to these and other important health benefits. With a new state administration, Kentucky has the opportunity to ramp up its efforts to get all Kentucky children covered, especially our youngest who are quickly being left behind.