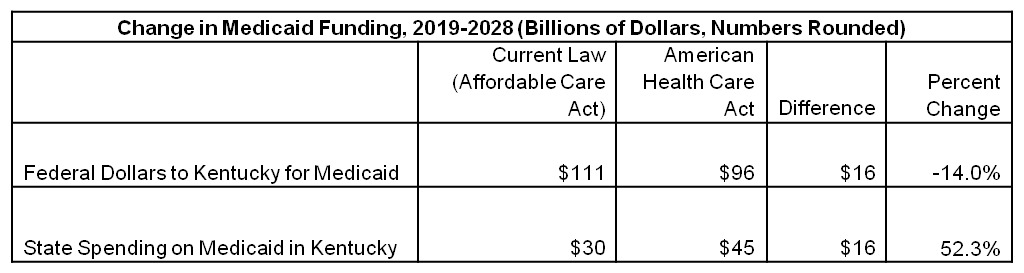
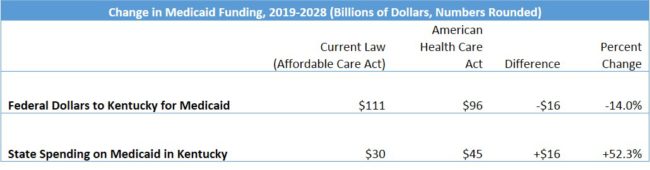
The House Republican plan to repeal and replace the Affordable Care Act (ACA), known as the American Health Care Act (AHCA), would cut federal funding for Medicaid in Kentucky by $16 billion over 10 years, according to an analysis by the Urban Institute. Making up that shortfall would require an increase in state Medicaid spending in Kentucky that would be bigger than all but one other state.
Cuts to Medicaid in the AHCA come in two ways. First, it would require Kentucky to spend approximately three times more than under current law to continue our Medicaid expansion. Second, it would further reduce federal dollars for Medicaid through changing the funding formula to what is called a “per capita cap.” Under that mechanism, federal funding will grow more slowly over time than Kentucky’s overall Medicaid costs.
According to the Urban Institute’s analysis, federal Medicaid spending in Kentucky would be 14 percent lower over the years 2019-2028 than it would be under the ACA, for a reduction in federal funding of $16 billion. State spending on Medicaid in Kentucky would have to increase 52.3 percent to fully make up for the federal cut, the biggest percentage increase of any state except New Mexico. States that have many low income people and that expanded Medicaid would have the biggest funding gaps to close.
Source: Urban Institute.
These estimates assume states do not cut Medicaid enrollment as a result of this cost shift. In reality, Kentucky would inevitably reduce eligibility, benefits and/or provider payments. The bill would effectively end Kentucky’s Medicaid expansion and squeeze funds for the traditional Medicaid program, which benefits children, people with disabilities and seniors. About 1.3 million Kentuckians currently receive Medicaid.
The Urban Institute’s analysis is based on the committee-approved bill and may be modified by further revisions to the legislation.