Kentuckians Are Concerned About Proposed Changes to Medicaid
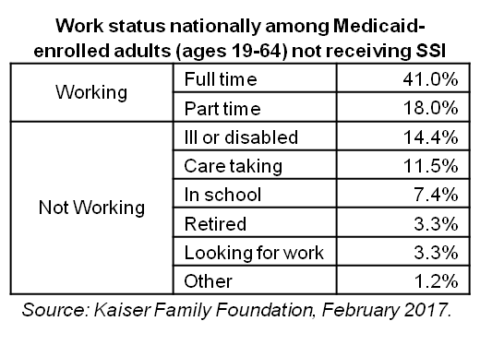
Kentucky officials recently asked the Centers for Medicare and Medicaid Services (CMS) to change certain parts of their original request...
Research That Works for Kentucky
Copyright © 2024 KyPolicy Privacy Policy Terms & Conditions Sitemap